by Dr. Bomi Joseph, Ph.D

__________________________________________________________________________________________________
Marijuana has been used as medicine for thousands of years but the use and consumption of it has changed dramatically, due to advances in genetics, cultivation and extraction processes. The potency of marijuana and cannabis concentrates has increased dramatically over the past 50 years, posing new potential risks and dangers that should be carefully considered.
This article is a neutral, scientific medical examination of marijuana. It is intended to help lawmakers and congressmen come up with a rational policy, nationwide.
__________________________________________________________________________________________________

A Brief History of Medical Cannabis Use
The therapeutic use Cannabis, has been known since ancient times. It was cultivated in China in 4000 BC, and is included in the oldest known pharmacopoeia, the Pen Ts'ao Ching, where it is recommended for "female’s disorders, gout, rheumatism, malaria, constipation and muscular weakness."1
In India, Cannabis is cited in Atharvaveda (II millennium BC) as "plant that releases anxiety". In Indian culture Cannabis plays an inconsistent role— a) as a plant sacred to Shiva, it is used as an intoxicant in popular religious rituals (“Holi”) and b) as a drug in various traditional medicines (i.e. Ayurveda, Unani, Tibbi).
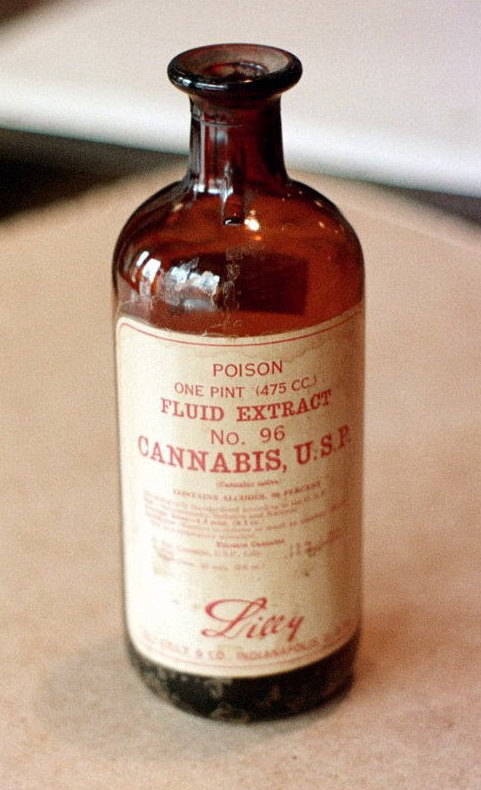
Between 1840 and 1900, more than 100 articles were published on medical uses of Cannabis as a potent narcotic, analgesic, hypnotic, treatment of convulsions, hysteria, depression and dysmenorrhea.” Cannabis was included on U.S. Dispensatory in 1854 with the following properties: "powerful narcotic.”2 It also mentions that it acts as an:
- aphrodisiac
- stimulates the appetite,
- occasionally induces a state of trance
- produces sleep
- relieves spasms
- calms nervous restlessness
- relieves pain.
As an analgesic, it differs from opium mostly because it does not decrease appetite, does not reduce secretions and does not cause constipation. Disorders which it was recommended are: neuralgia, gout, tetanus, hydrophobia, epidemic cholera, convulsions, chorea, hysteria, mental depression, insanity and uterine bleeding.
In 1860, Cannabis was so highly regarded that a "Committee on Cannabis indica" was formed by the Medical Association of Ohio. In the report published by the Committee (ed. RR M'Meens), Cannabis was recognized to treat tetanus, neuralgia, postpartum hemorrhage, childbirth pain, dysmenorrhea, convulsions, rheumatism, asthma, psychosis, post-partum depression, chronic cough, gonorrhea, chronic bronchitis, gastric pain, and more. In addition, it was found useful as a sleeping pill and as a drug that stimulates appetite. H.C.J. Wood reported that Cannabis indica was "used primarily for pain relief, to calm states of restlessness and malaise, to alleviate the suffering of incurable diseases, such as tuberculosis at the last stage, and finally as a mild sleeping pill."3
The world’s leading medical journal, The Lancet in 1887, recommended the use of Cannabis "night and day, and continued for some time" as “the best available remedy in the treatment of persistent headache.”4 More than twenty years later, William Osler, one of the fathers of modern medicine, believed the Cannabis to be "probably the most satisfactory remedy" for migraine,5 while J. Brown writes in the British Medical Journal that Cannabis "should have the first place in the treatment of menorrhagia.”6
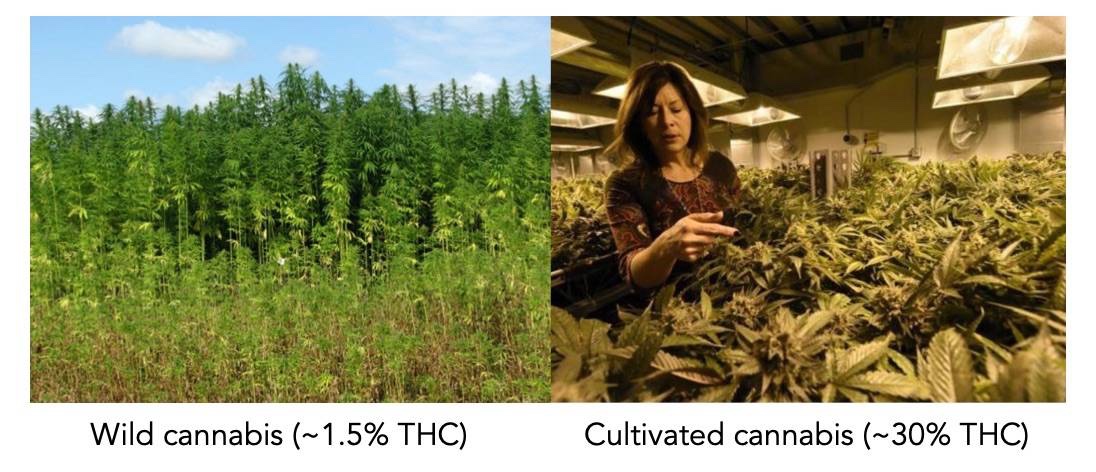
The federal government (National Institute of Drug Abuse or “NIDA”) awarded a contract (No. N01DA-15-7793 “Production, Analysis and Distribution of Cannabis, Marijuana Cigarettes and Related Materials”) to the University of Mississippi, in 2014. The cannabis they grow is the original Cannabis indica. This cannabis only has 1.3%-1.8% Tetra hydroxy cannabinol (THC), the active narcotic component of cannabis.
in 2015, a meeting of the American Chemical Society (ACS), in Denver, pointed out that the concentration of cannabis has risen by a factor of three in the last few decades. "As far as potency goes, it's been surprising how strong a lot of the marijuana is," said researcher and study lead Andy LaFrate. "We've seen potency values close to 30 percent THC, which is huge.”
The concentration of natural cannabis, in the wild, is around 1.5%. The concentration of illicit cannabis, sold in pot shops in the 1990s, was around 10% or less. But it has been bred upwards over the years, presumably because the market has demanded it. The "high grade" weed sold in dispensaries today has a potency of above 33%. The concentration of the cannabis oil, in its raw form, is about 50%. The concentration of the distillate can vary from 75% to 99%. The distillate is favored because it is “clean” and leaves no residue.
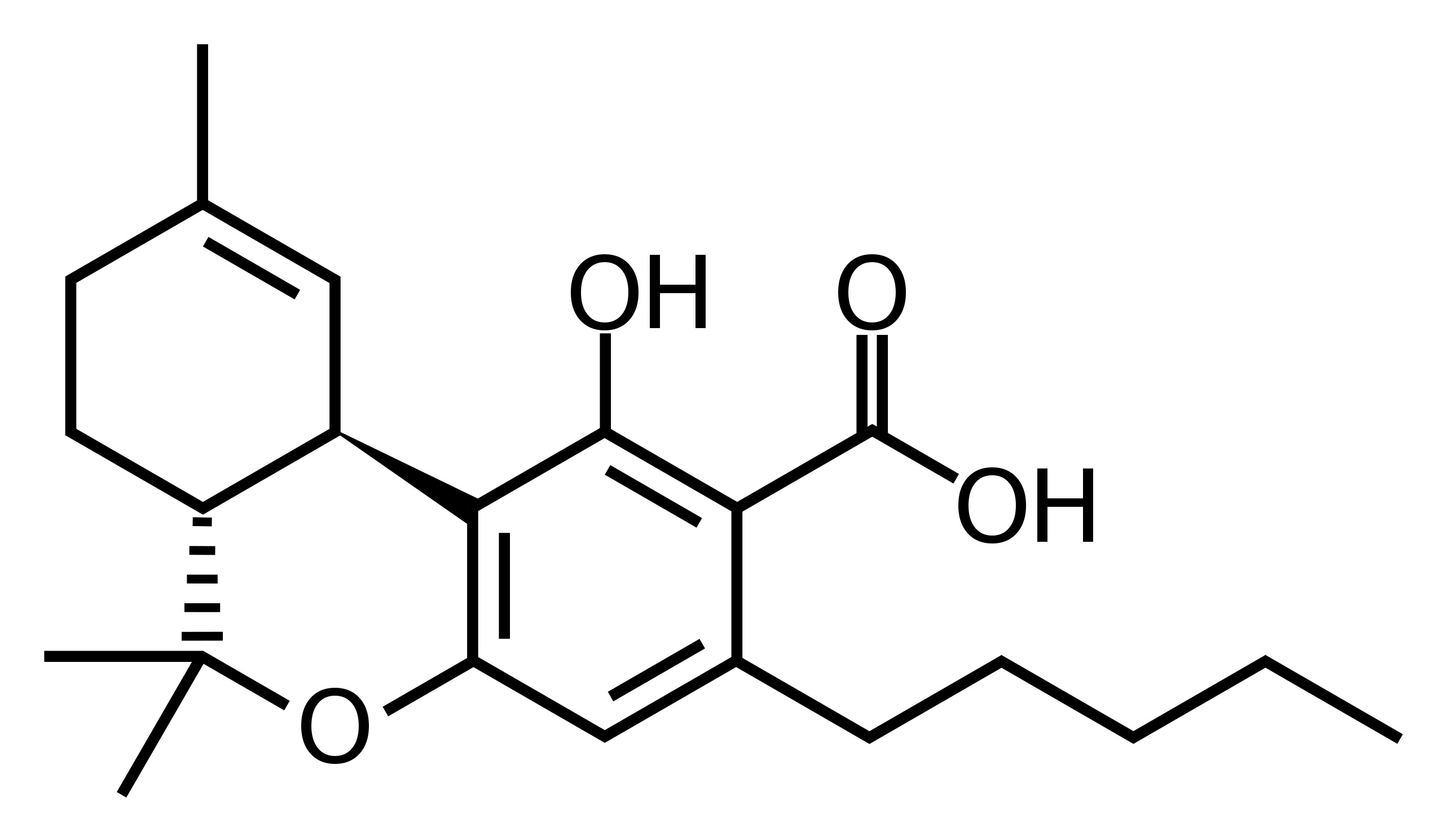
The true “medicinal” value of cannabis lies in a compound called CBD or “cannabidiol.” Natural cannabis, in the wild, has about 1.5% THC and also 1.3% CBD: almost a 1:1 ratio. The cannabidiol (CBD) content, in the genetically bred plant, has shrunk over time. The cannabis that has 30% THC only has about 0.3% CBD concentration, a 100:1 ratio. It means that people who rely on CBD properties for medicine, aren't getting much of it, irrespective of the medicinal claims of 30% THC cannabis.
The rise in THC content has been going on for years– but the steepness of the rise recently is greater than expected. “Although the rise in the concentration of THC is not a concern per se, the variability makes it more difficult to titrate the dose to the correct effect,” says Lewis Nelson, Professor and Vice Chair for Academic Affairs at NYU’s Department of Emergency Medicine and Director, of Medical Toxicology Fellowship at the New York City Poison Control Center. “This means that users are more likely to consume excessive doses, leading to adverse clinical effects. This has been seen already in Colorado emergency departments.”
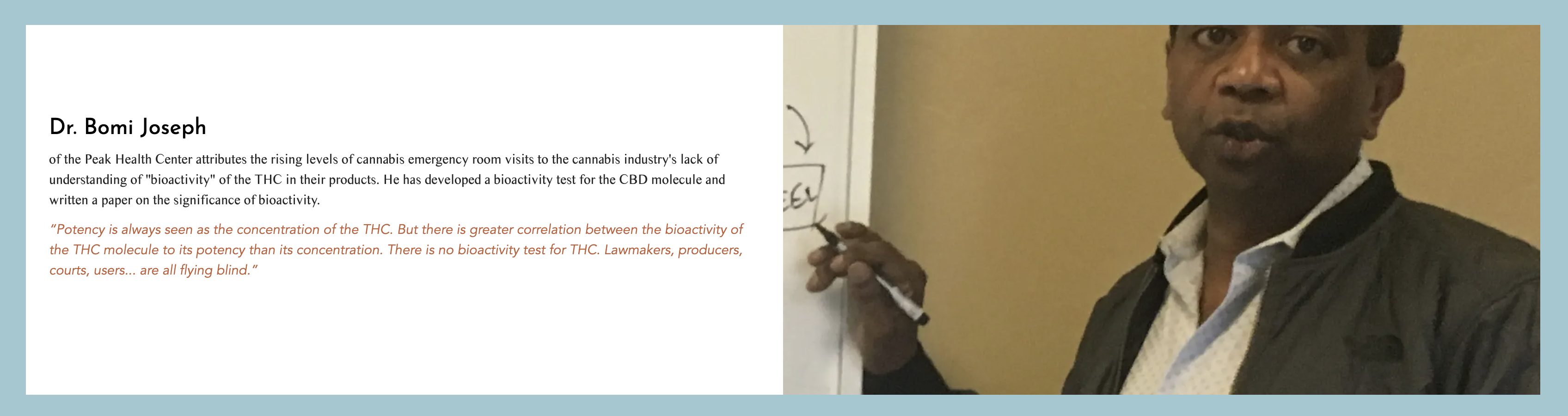
Nora Volkow, Director of the National Institute on Drug Abuse (NIDA) at the National Institutes of Health, agrees that it’s the higher THC content that’s driving the increase in marijuana-related emergency room visits in the country over the last several years. “The higher the THC content, the stronger the effects on the brain,” says Volkow, who's done research on this topic herself. “And the more likely you may end up with toxic reactions – like psychosis. Even the occasional user may end up in the ER. The very significant increase in ER visits – it's due to THC content being much higher now. It’s not that we’ve increased the number of people taking marijuana.”
She adds that the decline in CBD is concerning for medical reasons, since people who legitimately need its therapeutic effects may not be receiving them at all.
The changes in marijuana content are worth paying attention to, particularly given the gap between what's in the cannabis and what sellers are saying is in the cannabis. “Content labeling and dosing instructions would help,” says Nelson, “but accurate information may not be known by the grower or seller, highlighting the inadequate regulatory state of recreational and medical marijuana.”
Low-THC "Hemp" Flowers: Health Benefits Without the High
While THC levels have generally been increasing, there has been a trend in the opposite direction. Around 2010, cannabis seed banks started to stock high CBD strains with low levels of THC and around 2016 these started to be sold on the US consumer market as "hemp" flowers. In 2018 the Farm Bill was signed into law in the United States, legalizing possession & cultivation of industrial hemp which was defined by the law as containing less than 0.3% THC. There are now varieties of cannabis that contain between 12 to 24% CBD and less than 1% THC, offering substantial therapeutic properties with little-to-no "high" or side effects.

The "Blood Diamond" cannabis strain contains more than 24% CBD and less than 1% THC.
Some patients that the low-THC "hemp" strains can help with healthy inflammation, pain, sleep, appetite and mood without leaving them confused, groggy or "hungover" after the effects wear off.
Most patients should start off trying high-CBD "hemp" flowers, edibles or extracts first. Oftentimes these provide adequate relief. Moving up to stronger medical or recreational marijuana is often unnecessary.

High-THC Marijuana Impairs Driving, Low-THC "Hemp" May Not
According to a December, 2020 study published in the prestigious Journal of the American Medical Association, vaping high-THC and balanced (1:1) THC-to-CBD cannabis strains caused impaired driving, for up to 4 hours after consumption. When users vaped high-CBD cannabis ("hemp") strains that contained very little THC, their driving performance was not significantly or obviously impaired.7 This landmark study suggests that high-THC marijuana impairs driving and causes a higher risk of collision and that CBD may be a safer alternative.
"Safe" Levels of Cannabis Intake
Raw cannabis, in its natural form, has been chewed by humans for thousands of years. Raw cannabis has THCA, the acidic form of THC, and not THC. This is a mild narcotic, about 100 times milder than it’s well known cousin, Δ9-THC. Raw, leafy, cannabis has high chlorophyl and crude fiber content. It takes much longer for gastric enzymes to break down this product, and the milder THCA is released far more slowly into the blood stream.
When Cannabis is dried, THCA is converted into its “decarboxylated,” potent form called Δ9-THC. Indians call the natural, mild, form of dried cannabis flowers “bhang” and the more potent form of cannabis resin as “charas” (hashish).
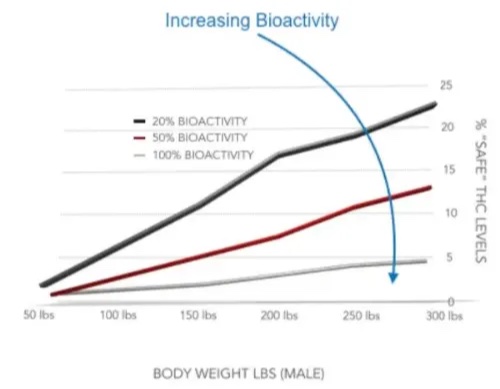
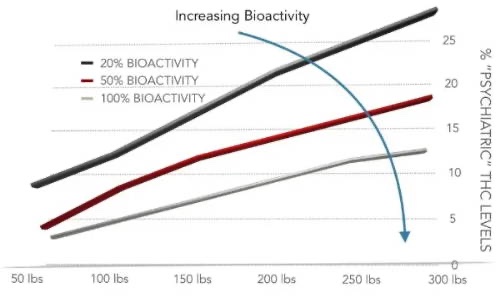
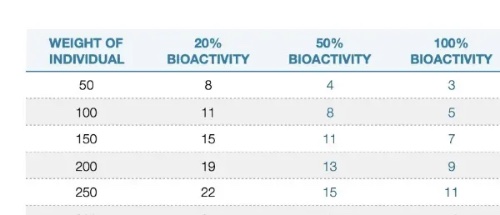
A “safe” level of THC is defined as the maximum concentration of Δ9-THC that an individual can consume, without exhibiting a significant somatic effect. The body weight of a human, and the bioactivity of the THC in cannabis, can make a ten fold difference in the “safe” level of THC! This can be seen in the above chart (this section) and it’s related data can be seen below:
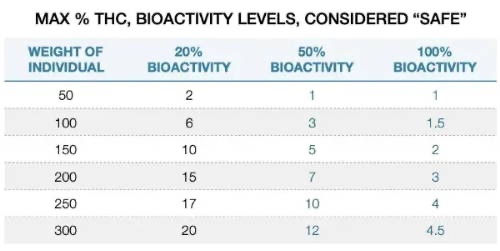
Levels Producing Somatic Effects
When the concentrations (and bioactivity) of THC are higher than the “safe” level, there are measurable short term physical effects. These include increased heart rate, dry mouth, reddening of the eyes (congestion of the conjunctival blood vessels), a reduction in intra-ocular pressure, involuntary muscle relaxation, sensation of cold or hot hands/feet and flushing of the face.8
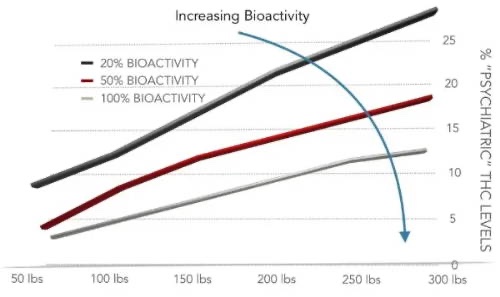
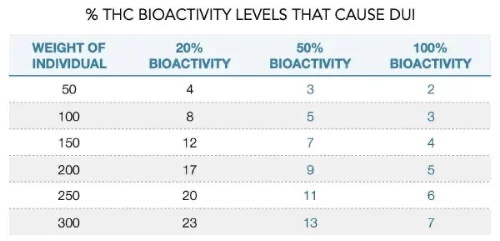
At these levels, Electroencephalography or EEG shows more persistent alpha brain waves that are of lower frequency than usual.9 Of particular importance to lawmakers and policy makers is that, at these levels, THC produces a "marked depression of motor activity."10 In other words, this is when people are “impaired” and “Driving Under the Influence” becomes a factor.
The visual representation of THC concentrations and bioactivity on DUI can be seen below (in this section). The tabular form, of the minimum concentration of Δ9-THC that affects an individual (exhibiting a significant somatic effect on the body) and causes DUI, can be seen below. As can be seen, the bioactivity of Δ9-THC is a significant factor in gauging safe levels of ingested THC.
Psychiatric & Addictive Effects of Cannabis
Medical professionals deal with the unintended consequence of marijuana legalization on a daily basis. The latest review of the American Journal of Health-System Pharmacy (2017) bluntly stated, “Marijuana legalization in Colorado has been associated with an increase in marijuana- related Emergency Department visits.”
The tip of a cigarette burns at 650o Celsius. Smoking is a fast way to get THC into the circulatory system. Smoking also denatures and reduces the bioactivity of THC. It is “tones down” the effects of THC but gives a “faster” high.
One of most problematic Marijuana-Related Emergency Department (MRED) visits is due to accidental pediatric intoxication. Children are particularly at risk from cannabis-containing food products, known as edibles, which look extremely similar to candy. The bioactivity and concentrations of these cannabis containing candies can be high. The chart above shows DUI causing levels of THC. 7 mg of 100% bioactive THC can spin a 300 lb man for a loop. Most candies have a “serving dose” of 10 mg THC. Imagine the effect that 10 mg of 100% bioactive THC will have on a 80 lb child!

Another cause of MRED visit is acute intoxication. Simply put, it refers to those who consume too much high bioactive THC. “The number of marijuana-related ED visits has nearly doubled since the drug’s use was legalized in Colorado,” authors wrote, “and the rate is higher for non-Colorado residents who are visiting the state.”
A study of 98 patients by the Mayo Clinic confirmed a new disease called Cannabinoid Hyperemesis Syndrome (CHS).11 It is a relatively new condition characterized by regular vomiting episodes. CHS, is associated with regular consumption of cannabis with THC concentrations above 26%. Cannabis has been consumed for thousands of years. CHS has appeared in MRED visits only after THC concentrations, in the dispensaries, have exceeded 25%. If the individual stops using cannabis, CHS usually reverses itself in 28 days.
Another worrisome source of MRED visits is due to “synthetic cannabinoids”. These are not natural cannabinoids but are chemical analogs intended to mimic the effects of natural cannabis. They have a high affinity for the CB1 receptor— a hundred to thousand times stronger than natural THC. These synthetic cannabinoids cause severe symptoms and also death. They are also called Spice, K2, Scooby Snax, etc.
Normal, “safe” marijuana is not supposed to be addictive. It is definitely not supposed to have psychiatric and addictive effects. Colorado voters legalized the sale and possession of limited amounts of marijuana for any purpose in 2012. Recreational stores began opening Jan. 1, 2014. Dr. Sam Wang studied teens who visited the emergency department in Denver, Colorado. He found that 111 teens and young adults visited Denver’s children’s emergency room for marijuana-related reasons in 2012. That number jumped to 631 in 2014, when the recreational dispensaries opened. Most worrisome is that a number of kids and young adults, in the emergency room for marijuana-related reasons, subsequently needed a psychiatric evaluations. This number increased rapidly — from 65 in 2012 to 442 in 2014. The patients who received psychiatric evaluations were found to be severely intoxicated or have tried to commit suicide or talked about committing suicide.
Some modern cannabis varieties contain more than 30% THC!
Modern, hybridized marijuana plants are genetic "freaks of nature!" This is not the normal profile for marijuana. Marijuana has been around for more than 6,000 years. It is only in the past 10 years, when the levels of THC has exceeded 15%, that most of the marijuana related complications and addictions have been reported.
The data, and the figures, for the various levels of bioactive THC that causes negative psychiatric and addictive effects are shown below:
Negative Effects of Marijuana on the Heart & Blood Vessels
Smoking is not good for you, period. Marijuana is sometimes touted as a safer, healthier alternative to smoking cigarettes but data suggests this is simply not true. A 2018 study published in Annals of Internal Medicine says that marijuana smoking diminishes the blood’s oxygen-carrying capacity 5x worse than tobacco smoking!12
In a 2020 study published in Journal of the American College of Cardiology, scientists concluded that there a wide range of risks to the heart and circulatory system associated with marijuana, in addition to many of the same risks as smoking tobacco.13 Among young patients suffering from their first heart attack, marijuana smoking was a common risk factor. The combination of cannabis smoking and pre-existing heart conditions is especially dangerous because inhaling particles of any type can be damaging to the heart and blood vessels.
Vaping cannabis isn’t safe because it delivers the compounds in the marijuana smoke more intensely and it causes increased doses to the heart. This means that the adverse effects are potentially more pronounced. It’s not just smoking and vaping that makes cannabis use dangerous. Even edibles can carry a certain amount of risk, especially when high amounts of THC are consumed.14
Marijuana activates the sympathetic nervous system and this causes the blood pressure to rise. This extra load on the heart which can be tougher for patients with pre-existing heart conditions to deal with. Anyone known to be at an increased risk of cardiovascular disease should be advised to cut down or quit their use of marijuana.

The Dangers of "Dabs" or High-potency Concentrates
Dabbing, or inhaling the hot vapor of high-potency cannabis extracts, has become a popular trend in the global cannabis culture. In some places where cannabis is legal, concentrates outsell dried marijuana. Different textures, grades & consistencies of cannabis extract go by various names such as: wax, shatter, live resin & budder. These frequently contain more than 70% THC and sometimes reach as high as 99% THC. If the extracts are from the black market, rather than regulated & meticulously quality-controlled sources, there is a real danger of contamination. In a 2015 study that tested 57 concentrate samples, over 80% were contaminated with residual solvents or pesticides.15

Users touch or “dab” small pieces of cannabis extract onto hot surfaces that are pre-heated with a blow-torch and then inhale the vapors through waterpipes called “dab rigs.” The psychotropic effects are extremely intense and can cause powerful euphoric, hallucinogenic & dissociative & schizophrenic effects, as well as “crashes” and hangovers after the effects wear off.16,17
Dabs Can Be Deadly!
In 2019, nineteen-year-old Colorado teenager Johnny Stack tragically took his own life after years of using high-potency cannabis extracts.18 Johnny was introduced to marijuana around the age of 15 and eventually he began dabbing and using concentrates which were legally available and heavily marketed to adults in his hometown of Denver. Friends and family say that he silently transformed from a normal, smart, charismatic teen to someone who became psychotic and delusional. "Little did we understand how concentrated some of the products are and how potent the weed is today, not like when we were kids," his mother Laura Stack said. "It’s so insidious. There are so many messages that kids hear: it's safe, it's legal, it must not be harmful. Their perception of it is so wrong!"
Dr. Rav Ivker, who is an advocate for CBD and medical cannabis, doesn't recommend dabbing for anyone. "There is no good medical reason to use anything that strong. With high doses of THC, it can potentially cause psychosis and schizophrenia. Our brain is not fully developed until we are in our mid-20s, it can be a problem," says Ivker.
Effects of High-potency Concentrates on the Endocannabinoid System
Chronic, high dosing of THC causes a predictable desensitization and downregulation of CB1 and CB2 cannabinoid receptors, accompanied by drug tolerance.
The degree of CB1 downregulation correlated with years of chronic cannabis smoking. CB1 densities returned to normal after four weeks of abstinence.19 Variable downregulation in different brain regions may explain why frequent users of cannabis develop tolerance to some effects of THC, such as anxiety and cognitive impairment, but not to its euphoric effect.
Johnny Stack, R.I.P.
My Proposed "Rational Policy" on Cannabis Potency
This recommendation is based on the fact that smoked THC has a lower bioactivity than ingested, edible THC.
Recreational Use of Marijuana
- The limit for “recreational” use of marijuana, for smoking or vaping, be a maximum concentration of 5%. This is a safe upper limit that rarely causes addiction or psychoses. It also has minimal, trace, or no somatic side effects.
- Low-dose edibles are a healthier way to consume cannabis than smoking or vaping. The limit for “recreational” use of marijuana, for edibles, be a maximum concentration of 3%. The maximum amount per serving size be limited to 2 mg THC. The daily limit for recreational edibles be 4 mg THC, or not more than 2 servings per day (if the amount per serving is 2 mg).
- This low concentration, and low limit of THC, brings the cannabis consumption closer to historical levels of use of natural cannabis. This may assuage the concern of federal officials and make them more amenable to “recreational” use of marijuana.
- The only variable that the industry can tinker with, to increase the potency of recreational use of marijuana, is the bioactivity of THC.
- The industry, and the users, will have to adjust. Other than NIDA’s farm at the University of Mississippi, there are almost no plants and products available with such low levels of THC in USA.
Medical Use of Marijuana
- The limit for “medicinal” use of marijuana, for smoking or vaping, be a maximum concentration of 15%. Although tame by todays standards, this is a high upper limit. It is more than enough to significantly impair motor skills, and cause DUI. It causes noticeable somatic effects.
- All “medicinal” marijuana products should have a CBD:THC ratio of at least 1:3. If a medicinal marijuana product, sold for smoking, has a THC concentration of 15%, it should have a CBD concentration of at least 5%. If it has a “medicinal” claim, it should at least have the active ingredient in the medicine.
- The limit for “medicinal” use of marijuana, for edibles, be a maximum concentration of 5%. The maximum amount per serving size be limited to 5 mg THC. The daily limit for medicinal edibles be 10 mg THC, or not more than 2 servings per day (if the amount per serving is 5 mg).
- This concentration, is high enough to be medicinal— in a significant way. It is high enough to cause somatic effects and cause DUI. But it is not high enough to be widely addictive or cause psychiatric problems. It will reduce marijuana related emergency department (MRED) visits (other than synthetic marijuana related visits).
- Medicinal marijuana be prescribed by a licensed physician and the physician’s prescriptions be tracked in a independent database, as drug registry is currently done. This allows the authorities to be notified automatically when a physician is rampantly prescribing medicinal marijuana. There can be limits also set on a physicians ability to prescribe medicinal marijuana.
- The only variable that the industry can tinker with, to increase the potency of medicinal use of marijuana, is the bioactivity of THC.
The Bottom Line
We should ban the all forms of marijuana above 20% THC: flowers, leaf trim, oils, concentrates & edibles, etc.
There is no medical reason to have THC levels above 20%.
There is only a significantly increased risk of addiction, psychiatric problems & physical & mental degradation!
Final Thoughts
The final two points are extremely important to consider:
- The bioactivity of the THC molecule is a vital piece of information that needs to be known. We have the technology and the ability to develop a test that measures the bioactivity of THC. Because of the stigma associated with the federal ban on THC, private investors are loathe to fund the development of the THC bioactivity test.
- It is quite straightforward for regulators to tax, or appropriate cannabis-derived tax revenue to the development of the bioactive THC molecule. This is a crucial missing link in the ability to regulate, or even measure intoxication levels for producers, prosecutors and lawmakers.
.:: References ::.
- H.L. Li, Econ. Bot. 28 (1974) 293-301.
- G.B. Wood and F Bache. The dispensatory of the United States, Philadelphia, Lippincott, Brambo & Co. 1854.
- H.C.J. Wood in Treatise on Therapeutics (6th ed.) Philadelphia, J.B. Lippincott & Co. 1886.
- Letter from London: The Lancet, December 3, (1887) 732.
- W. Osler, T. McCrae in The principles and practice of medicine (8th ed.) New York, D. Appleton & Co. 1912.
- J. Brown, Brit. Med. J. 1 (1883) 1002.
- JAMA. 2020;324(21):2177-2186.
- Moelker, Wendy (19 Sep 2008). "How does Marijuana Affect Your Body? What are the Marijuana Physical Effects?”
- Kalant, H.K.; Roschlau, W.H.E. (1998). Principles of Medical Pharmacology (6th ed.). pp. 373–375.
- Andersson, M.; Usiello, A; Borgkvist, A; Pozzi, L; Dominguez, C; Fienberg, AA; Svenningsson, P; Fredholm, BB; Borrelli, E; Greengard, P; Fisone, G (2005). "Cannabinoid Action Depends on Phosphorylation of Dopamine- and cAMP-Regulated Phosphoprotein of 32 kDa at the Protein Kinase A Site in Striatal Projection Neurons". Journal of Neuroscience. 25 (37): 8432–8. PMID 16162925. doi:10.1523/JNEUROSCI.1289-05.2005
- Simonetto, Douglas A.; Oxentenko, Amy S.; Herman, Margot L.; Szostek, Jason H. (2012). "Cannabinoid Hyperemesis: A Case Series of 98 Patients". Mayo Clinic Proceedings. 87 (2): 114–9. PMC 3538402 . PMID 22305024. doi:10.1016/j.mayocp. 2011.10.005.
- Ann Intern Med. 2018 Feb 6; 168(3): 187-194.
- J Am Coll Cardiol. 2020 Jan 28;75(3):320-332.
- J Clin Med 2020, 9(6),1925;
- J Toxicol Sci. 2015 Dec;40(6):797-803.
- Addict Behav. 2014 Oct;39(10):1430-3.
- Schizophr Res. 2016 Apr;172(1-3):211-2.
- Glasgow, John. “Family Who Lost Son to Suicide Calling on State for THC Potency Limits.” 9News, KUSA-TV, 26 November 2020, www.9news.com/article/news/local/mile-high-mornings/family-wants-thc-potency-limits/73-ebe2c5e9-f2cf-4288-8db7-2183c19d8acf.
- PLoS One. 2014;9(3): e89566.
